Telomeres are structures responsible for the maintenance of chromosomal stability. Telomere length is maintained by the telomerase complex, shelterin proteins, and others involved in telomere biology. Germline variants in telomere-biology genes may cause excessive telomere shortening, cell senescence, and genomic instability, which in humans may clinically translate into bone marrow failure, liver and lung fibrosis, skin lesions, and a proclivity for cancer. The prevalence of telomere diseases is unknown, partly due to variable penetrance. Patients without phenotypical signs or a family history may be misdiagnosed as having acquired aplastic anemia (AAA). Other inherited bone marrow failure syndromes (IBMF) and AAA may also present with short telomeres.
The aim of this study was to determine the genetic variants in patients with bone marrow failure (BMF) and short telomeres. The study was conducted at a tertiary hospital in Sao Paulo, Brazil. One-hundred forty-four patients with BMF followed between 2016 and 2022 were enrolled. Ethical approval was obtained from the local Ethics Committee. Telomere length was determined by Southern blot or flow-FISH in peripheral blood leukocytes. Telomeres were interpreted as short when below the 10th percentile according to age. All samples were submitted to genomic analysis by Next Generation Sequencing (NGS), using a panel for 154 genes associated with hematologic malignancies and BMF syndromes.
A presumptive diagnosis was made based on clinical and laboratorial data. Liver or pulmonary fibrosis, early greying, dystrophic nails, leukoplakia, hypopigmented skin, solid malignant tumors, retinopathy, family history of hematological diseases and consanguinity were considered as red flag symptoms for telomeropathies. Patients with no red flags who had severe cytopenias were considered as having possible AAA. Patients with non-severe cytopenias starting at an early age were considered as possibly having other IBMF syndromes.
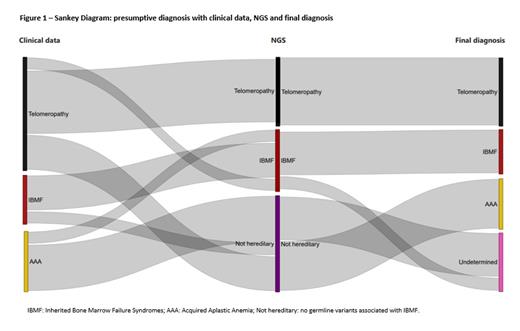
Thirty patients (21%) out of 144 analyzed had short telomere length and were included. They had their telomeres measured at diagnosis (53%) or at follow-up (47%).Combining clinical, laboratory, and NGS data, 10 patients (34%) were diagnosed with Telomeropathies [TERT (N=4), RTEL1 (N=3), DKC1 (N=1), TERC (N=1), ACD (N=1)]. Six patients (20%) were diagnosed with other IBMF syndromes [4 Fanconi anemia (FANCA, FANCG, BRCA2), 1 GATA2 deficiency (GATA2), 1 Blackfan-Diamond anemia (RPS19)]. Seven patients (23%) were considered as having AAA, not having any germline variants, and 7 (23%) as undetermined cases, with some suggestive clinical feature but no identified germline variant (figure 1). Comparing with NSG data, the clinical and laboratorial presumptive diagnosis had a 95% accuracy, 100% sensitivity and 92% specificity.
In the group with confirmed telomeropathy (N=10), 70% were male, 80% were white, and the median age at diagnosis was 25 years. All of them had at least one red flag symptom: hepatic fibrosis (60%), early graying (60%), family history of hematologic diseases (40%) and one patient had the classic dermatologic triad of dyskeratosis congenital. Only one had severe cytopenia and none had significant paroxysmal nocturnal hemoglobinuria clone. Most of them had hypoplastic bone marrow without significant dysplasia (N=8).
In conclusion, clinical features combined with laboratory analysis had high accuracy when compared with NGS. Despite having access to NGS, a final diagnosis was not achieved for 23% of patients, who would benefit from further genetic analysis.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal